
With the health needs of the Filipino people as its prime consideration, the Department of Otolaryngology - Head and Neck Surgery of the University of the Philippines - Philippine General Hospital (UP-PGH) has been actively involved in service, teaching, training, and research - all aiming to improve the practice of Otolaryngology - Head and Neck Surgery, and prioritize providing exemplary service and efficient health delivery.
The Department comprises different divisions headed by highly trained and competent specialists. These are the following:
- Otology, Neurotology, Audiology, and Lateral Skull Base Surgery
- Rhinology, Paranasal Sinus, and Anterior Skull Base Surgery
- Laryngobronchoesophagology and Neck Surgery
- Oral Cavity, Oropharynx, Salivary Gland, and Sleep Surgery
- Craniomaxillofacial Plastic and Restorative Surgery
- Head and Neck Surgery
Vision
The Department of Otorhinolaryngology, University of the Philippines – Philippine General Hospital shall be an internationally recognized center of excellence in the field of Otorhinolaryngology – Head and Neck Surgery.
Mission
The health needs of the Filipino people shall be its prime consideration. It shall provide excellence and leadership in the field of Otorhinolaryngology – Head and Neck Surgery by teaching, providing exemplary clinical practice and dynamically pursuing relevant researches beneficial to the community in an environment guided by moral, ethical and spiritual values.
The specialty of Otorhinolaryngology has its beginning in the specialty formerly known as EENT – Eyes, Ears, Nose and Throat. The Department was organized in May 1911 and was headed by Dr. Reinhert Rembe, a naturalized American of German ancestry. Within two years of its inception, the department began admitting resident physicians.
When Dr. Rembe left the Philippines in 1914, Dr. Aristeo Rizal Ubaldo, assistant head, took over management of the Department. Around the time of his chairmanship, Dr. Ubaldo toured famous eye, ear, nose and throat clinics of Europe and returned with an instrument called the Barraquer’s Erisophake. With this, Dr. Ubaldo introduced intracapsular cataract lens extraction in the country — a milestone in Philippine Ophthalmology. This was followed by other great achievements such as the first laryngectomy by Dr. Ubaldo and Dr. Antonio S. Fernando, Sr. in 1923 and the introduction of the first bronchoesophagology clinic by Dr. Vivencio C. Alcantara in 1932.
With rapid developments within the specialty of EENT, there was a call for its separation into two distinct specialties. In 1961, the University of the Philippines Board of Regents granted autonomy to the Department of Otorhinolaryngology, effectively separating it from the Department of Ophthalmology. Thereafter, the Department of Otorhinolaryngology (ORL) began its exodus into the specialty that it is today. Dr. Carlos Yambao, the department’s first Chair, and his colleagues paved the way for further development of the field.
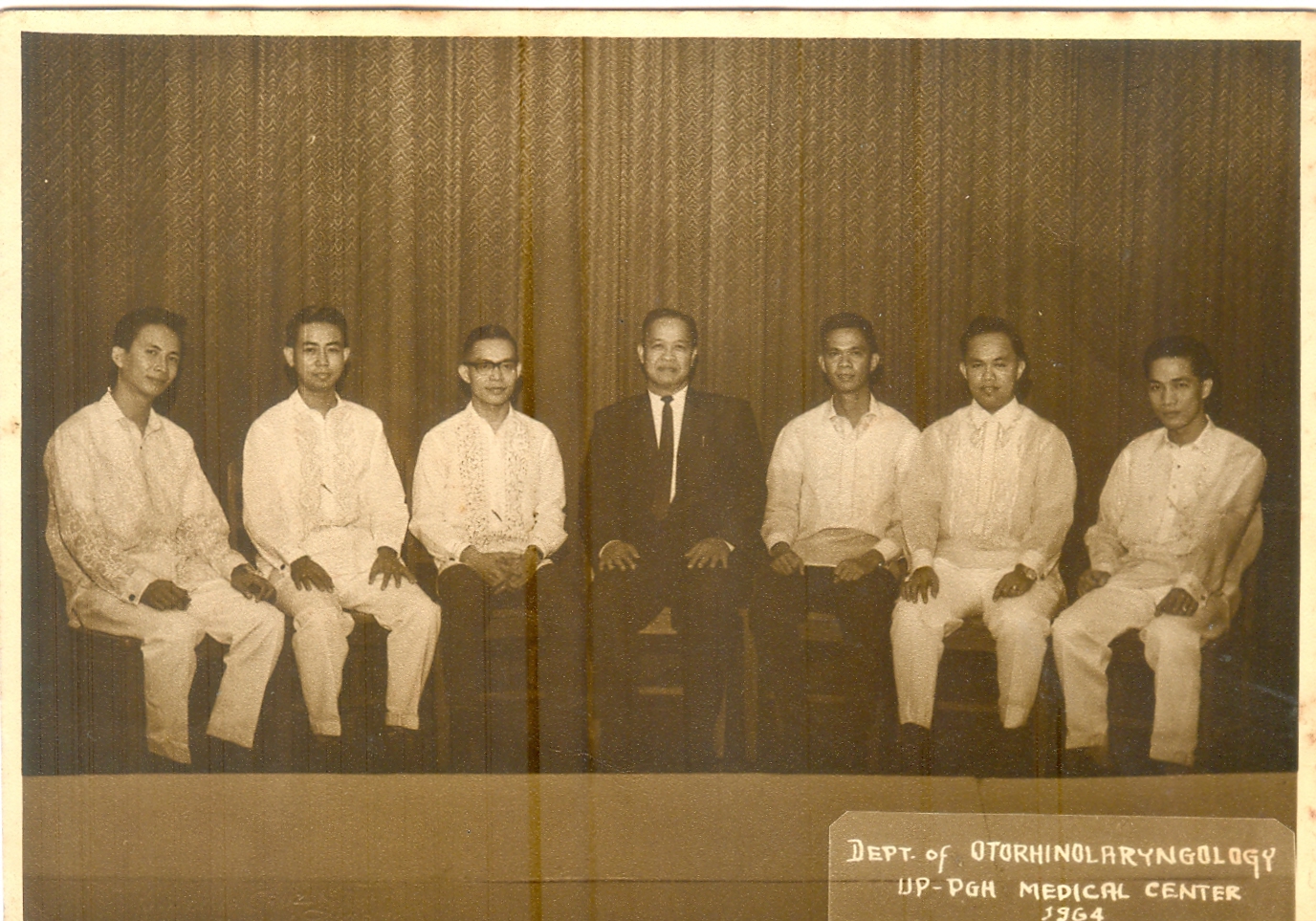
1964 Medical Staff with Chairman Dr. Yambao in the center
The next few decades saw successive milestones that allowed for further expansion of the Department. Dr. Tierry F. Garcia saw the expansion of the specialty to include Head and Neck Surgery. Dr. Mariano B. Caparas embarked on a faculty development program that encouraged consultants to pursue post-graduate fellowships, thereby improving upon residency training with their return. Dr. Caparas also saw the establishment of an Instrument Design Section and the creation of the Prosthesis Unit, paving the way for resourcefulness even in the setting of scarcity. Dr. Armando Chiong Sr. established the ORL Library, emphasized the importance of research, and oversaw the creation of Study Groups. His time as chair saw the creation of the Ear Institute, which has since then evolved into the Philippine National Ear Institute. Dr. Manuel Lim steered the completion of the Temporal Bone Dissection Laboratory, and conceived the idea for the Ear Research and Training Center, known also as the Ear Unit. Dr. Edilberto Jose headed the modernization of equipment, allowing further training in endoscopic and microscopic techniques. Dr. Joselito Jamir directed the publication of the Textbook of Basic Otolaryngology, and it was during this period that the two-track residency program which allowed for obtaining masteral degrees together with residency training was established. The MS Clinical Audiology program was also initiated at this time. Dr. Generoso T. Abes facilitated the continued evolution of the Ear Unit, and promoted the creation of the first cochlear implantation program in the Philippines. It was during this time as well that the Head and Neck Fellowship Program was created. Dr. Rene S. Tuazon emphasized the primary role of teaching as the UPCM shifted to an Organ System Integration (OSI) curriculum, and the multidisciplinary approach to patient care was coupled with the launch of an ORL Information System. Dr. Alfredo Q. Pontejos, Jr. fostered a growing interest in research, which led to increased trainee and faculty participation in both local and international conferences. Dr. Josefino G. Hernandez led the Department through the challenges of the COVID-19 pandemic, prioritizing a balance of safety for the wellbeing of trainees, faculty, and staff, without compromising quality training and provision of essential Otolaryngology services to patients. Dr. Maria Rina Reyes T. Quintos - the current Chair, continues to lead the Department as it further pushes for excellence in the the fields of training, education, research, and service.
Prosthesis Unit in the 1990s
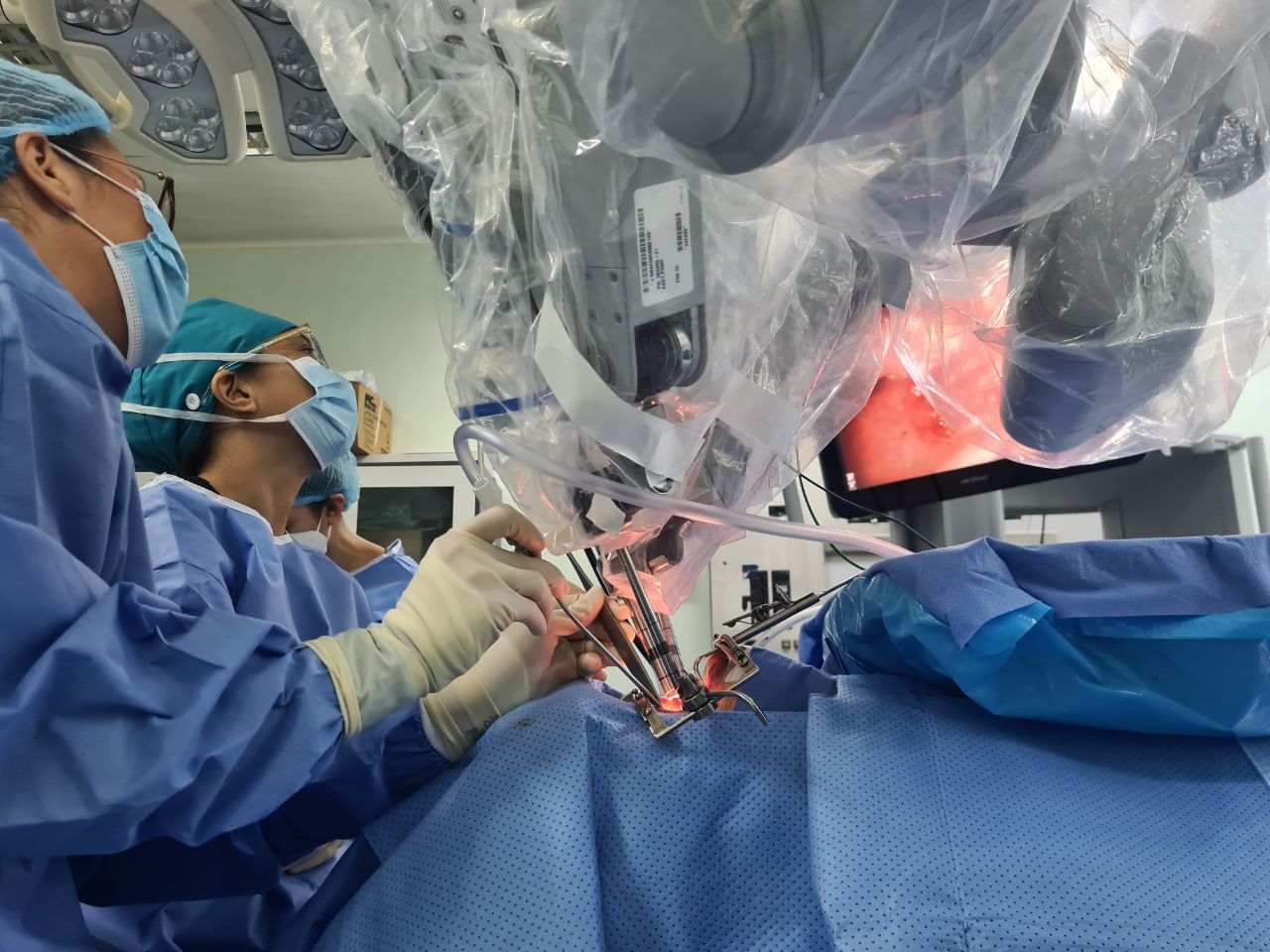
At present, the Department has been continuously adapting to fast-paced developments in the field of Otolaryngology - Head and Neck Surgery. It has acquired new equipment - top of the line Zeiss operating microscopes, CO2 and KTP A.R.C laser machines, the new Spies Rhinology tower, and new microlaryngeal surgery and bronchoscopy sets. The acquisition of the Da Vinci Robotic Surgical System has allowed for even greater access to complex surgical procedures. The residency training program has also been continuously adapting to the newly-recommended Outcome-Based Education (OBE) requirements of the Philippine Board of Otolaryngology, Head and Neck Surgery which has further increased the number of alternative teaching strategies, improved the quality of consultant supervision in operative procedures and outpatient clinics, and provided more objective and constructive assessment of residents’ performance.
Four-Year Accredited Residency Training Program
The residency training program of the Department of Otolaryngology - Head and Neck Surgery is a four-year Philippine Board of Otolaryngology - Head and Neck Surgery accredited training program with subspecialties comprising the different divisions described below:
| Divisions | Divisions Head |
| Rhinology, Paranasal Sinus and Anterior Skull Base Surgery | Ramon Antonio B. Lopa, MD |
| Craniomaxillofacial, Plastic, and Restorative Surgery | Philip B. Fullante, MD |
| Oral Cavity, Pharynx, Salivary Gland, and Sleep Surgery | Agnes T. Remulla, MD |
| Laryngobronchoesophagology and Neck Surgery | Ryner Jose C. Carrillo, MD, MSc (Clin Epi) |
| Head and Neck Surgery | Jeannette Marie S. Matsuo, MD |
| Otology, Neuro-otology, Audiology and Lateral Skull Base Surgery | Nathaniel W. Yang, MD |
Residents are evaluated in four areas: 1) knowledge, 2) clinical and surgical skills, 3) attitude, and 4) research output. Knowledge is measured by monthly in-house exams by the training officer and chief resident, residents are conducted during the last quarter of year. Clinical and surgical skills are evaluated by consultant’s assessment through appropriate grading materials, recommended by the PBO-HNS. Residents’ researches are likewise evaluated during various research activities (Interesting Case Contest, Descriptive Research Presentation, Analytical Research Presentation, regular research updates).
Head and Neck Oncology Surgery Fellowship Program
The Head and Neck Surgical Oncology Fellowship program of the department is a one-year high volume, clinical fellowship program geared towards producing subspecialists in the field of head and neck tumor/cancer treatment and care. The program aims to develop a head and neck surgeon who has a holistic grasp in the management of head and neck tumors/cancers with emphasis in training the fellow in performing difficult and complicated tumor surgeries in the head and neck. The fellowship program prides itself in elevating the treatment of head and neck cancers towards a multidisciplinary approach to involve other specialties to improve the outcomes of our patient care. Every Wednesday, for more than 20 years, this multidisciplinary team of specialists from Radiation Oncology, Medical Oncology, Pathology, Radiology, Psychiatry, Palliative and Hospice Care and our Head and Neck Surgical Oncology team meet and discuss the best treatment plans for head and neck tumor/cancer patients from initial care to post treatment surveillance. The program has produced numerous graduates who are now practicing in different parts of the country, operating and treating head and neck tumor/cancer patients in their localities.
Craniomaxillofacial Prosthesis Fellowship Program
The craniomaxillofacial fellowship program of the Department is a two-year fellowship program that starts during the second year of residency for two residents interested in developing skills and the discipline in fabricating and providing prosthesis for patients suffering from post-operative head and neck defects. The fellows are trained to fabricate prosthesis that help patients regain their normal speech after surgical removal of the palate or fabricate a prosthetic nose for patients whose noses had to be removed because of cancer among others. Aside from these, the fellows create prostheses for cleft lip and palate patients to prepare and optimize these patients for their eventual definitive surgeries.
Philippine Academy of Facial Plastic and Reconstructive Surgery (PAFPRS), Rotating Fellow
The Philippine Academy of Facial Plastic and Reconstructive Surgery (PAFPRS) works with UP-PGH ORL-HNS in having their fellowship trainees rotate in the Department for several months to perform selected surgeries, observe in facial and reconstructive surgeries, and participate in the weekly ORL-HNS Facial Plastic rounds, multidisciplinary tumor board, and grand rounds. The fellows, in turn, present a quarterly audit consisting of a census of cases seen and surgeries performed.
Master in Clinical Audiology Program
The Masters in Clinical Audiology program was started in May 1999 and is offered every two years. Students spend their time in the Ear Unit for eight (8) hours a week to perform the different diagnostic tests on different patients, in addition to their classes. Faculty members come from the Department of ORL-HNS and the Department of Speech Pathology University of the Philippines College of Allied Medical Professions. Students are trained with full hands-on laboratory work, and the program allows integration of audiologic diagnosis and hearing aid analysis into the existing training program. The program also benefits from the upgraded Temporal Bone Dissection Laboratory and Vestibular Laboratory. Graduates of the Master of Clinical Audiology and ORL-HNS residency programs acquire skills for audiologic diagnosis and rehabilitation when they leave the hospital.
Post-Graduate Courses
Post-graduate courses, lectures and seminars strengthen the residents’ understanding of the concepts essential to the specialty and provide much needed avenues to discuss management and treatment protocols with experts in the field. The basic thrust of the department has always been excellence in the field of Otorhinolaryngology – Head & Neck Surgery through teaching and training of both residents and medical students. Residents are involved in the teaching process and play a role in producing teaching aids such as the Self-Instructional Learning Modules for UP College of Medicine students.
Enumerated in the list that follows are the annual postgraduate courses conducted by the department and open to other trainees from other institutions:
- Functional Endoscopic Sinus Surgery Course - held yearly
- Functional Rhinoplasty Course - held yearly
- Images in ENT (Clinicoradiologic Correlation) - held every two years
- Basic Head and Neck Course- held every two years
- In-house Temporal Bone Dissection Course - held yearly
- Temporal Bone Dissection Course (open) - held yearly
MARIA RINA T. REYES-QUINTOS, MD, MClinAud, PhD
Chair
JEANNETTE MARIE S. MATSUO, MD
Executive Officer and Vice Chair for Administration and Support Services
AGNES N. TIRONA-REMULLA, MD
Vice Chair for Undergraduate Training and Graduate Programs
ARSENIO CLARO A. CABUNGCAL, MD
Vice Chair for Postgraduate Training
RAMON ANTONIO B. LOPA, MD
Vice Chair for Patient Services
KIMBERLY MAE C. ONG, MD, MSc
Vice Chair for Research
ANNA PAMELA C. DELA CRUZ, MD
Training Officer

Faculty Members during the Department Annual Photoshoot

Faculty Members, together with some of the Department staff, during the 2025 Strategic Planning
| Faculty Name | Degree | Rank |
| Abes, Generoso T. | MD, MPH | Professor Emeritus |
| Alzaga, Jennifer Angela A. | MD | Medical Specialist III, PGH with Teaching Assignment |
| Arquiza, Christine Joy S. | MD, MS Health Informatics | Clinical Associate Professor, UP College of Medicine and Attending Otorhinolaryngologist, PGH, Medical Specialist III PGH |
| Baligod, Genilou Liv J. | MD | Attending Otolaryngologist, PGH |
| Bautista, Reinzi Luz S. | MD | Attending Otolaryngologist, PGH |
| Cabungcal, Arsenio Claro A. | MD | Assistant Associate Dean for Planning and Development, UP College of Medicine. Associate Professor 5, UP College of Medicine and Attending Otolaryngologist, PGH |
| Calaquian, Christopher Malorre E. | MD | Clinical Associate Professor, UP College of Medicine and Attending Otorhinolaryngologist, PGH Medical Specialist III, PGH |
| Carrillo, Ryner Jose D. | MD, MS (Clin Epi) | Clinical Associate Professor, UP College of Medicine and Attending Otorhinolaryngologist, PGH Professor 4, Dept. of Anatomy, College of Medicine |
| Chan, Abner L. | MD | College Secretary, UP College of Medicine. Professor 4, UP College of Medicine and Attending Otorhinolaryngologist, PGH |
| Chiong, Armando Jr., M. | MD | Clinical Associate Professor, UP College of Medicine and Attending Otorhinolaryngologist, PGH Medical Specialist III, PGH |
| Chiong, Charlotte M. | MD, PhD | Dean, UP College of Medicine. Clinical Professor, UP College of Medicine and Attending Otolaryngologist, PGH. Research Professor 12, National Institutes of Health, UPM |
| Cruz, Teresa Luisa G. | MD, MHPEd | Associate Dean for PGIM, UP College of Medicine, Professor 4, UP College of Medicine and Attending Otorhinolaryngologist, PGH |
| Dela Cruz, Anna Pamela C. | MD | Clinical Associate Professor, UP College of Medicine and Attending Otolaryngologist,PGH |
| Fellizar-Lopez, Kathleen Makrina R. | MD, MPH | Clinical Associate Professor, UP College of Medicine and Attending Otorhinolaryngologist, PGH |
| Fernandez, Rodolfo Uy III U. | MD | Attending Otolaryngologist, PGH |
| Fullante, Philip B. | MD | Clinical Associate Professor, UP College of Medicine and Attending Otolaryngologist, PGH, Medical Specialist III PGH |
| Hernandez, Josefino G. | MD | Professor 2, UP College of Medicine and Attending Otolaryngologist, PGH |
| Hernandez, Melfred L. | MD, MHA | Associate Professor 4, UPM Associate Professor 4, UP College of Medicine and Attending Otolaryngologist, PGH |
| Lapeña, Jose Florencio Jr., F. | MA, MD | Professor 12, UP College of Medicine and Attending Otolaryngologist, PGH |
| Llanes, Erasmo Gonzalo D.V. | MD, MSc in Epidemiology (Public Health) | Clinical Associate Professor, UP College of Medicine and Attending Otolaryngologist, PGH |
| Lopa, Ramon Antonio B. | MD | Associate Professor 3, UP College of Medicine and Attending Otolaryngologist, PGH |
| Matsuo, Jeannette Marie S. | MD | Clinical Associate Professor, UP College of Medicine and Attending Otolaryngologist, PGH Medical Specialist III, PGH |
| Ong, Kimberly Mae C | MD | Attending Otolaryngologist, PGH; Research Assistant Professor I |
| Pontejos, Alfredo Quintin Y., Jr. | MD | Clinical Professor, UP College of Medicine and Attending Otolaryngologist, PGH |
| Porquez, John Michael G. | MD | Attending Otolaryngologist, PGH |
| Reyes-Quintos, Maria Rina T. | MD, MClinAud, PhD Medical Sciences | Clinical Associate Professor, UP College of Medicine and Attending Otolaryngologist, PGH Research Professor 3, National Institutes of Health, UPM |
| Reyes, Ronaldo A. | MD, DMD | Clinical Associate Professor, UP College of Medicine and Attending Otolaryngologist, PGH, Medical Specialist III, PGH |
| Ricalde, Rosario R. | MD | Clinical Associate Professor, UP College of Medicine and Attending Otolaryngologist, PGH Research Assistant Professor 4, Philippine National Ear Institute |
| Tantoco, Ma. Leah C. | MD | Attending Otolaryngologist, PGH |
| Tirona-Remulla, Agnes N. | MD | Associate Professor 3, UP College of Medicine and Attending Otolaryngologist, PGH |
| Villafuerte, Cesar Vincent III L. | MD | Clinical Associate Professor, UP College of Medicine and Attending Otolaryngologist, PGH, Research Assistant Professor 3 |
| Yang, Nathaniel W. | MD | Associate Professor 5, UP College of Medicine and Attending Otolaryngologist, PGH |
Craniomaxillofacial Prosthesis and Bioengineering Unit
The Department has its own laboratory that fabricates cranio-maxillo-facial prosthetics. Prosthetic devices fabricated in the unit consists of feeding/ molding plates for cleft lip and palate patients; surgical, interim and permanent obturators for post-maxillectomy patients; occlusal splints, and lingual splints to name a few. Facial, nose and ear prostheses are also made here for patients who need these. The Department is closely affiliated with the University of the Philippines Surgical Innovation and Biotechnology Laboratory (UP SIBOL), which aims to provide quality and affordable medical devices to patients.
Ear Unit
The Ear Unit is officially under the Philippine National Ear Institute. It functions as a service provider for the hospital in hearing examinations such as otoacoustic emission, auditory brainstem response, pure tone audiometry, speech testing, tympanometry and hearing aid fitting. It also offers tests for vertigo and balance which are only available in very few institutions, like the video head impulse test (VHIT) and cortical evoked potential. The Ear Unit likewise functions as a venue for training of the department’s residents and students of the Masters in Clinical Audiology of the UP College of Medicine in conducting the above-mentioned tests.
Videostroboscopy Unit
This unit is equipped with a laryngeal videostroboscopy machine and serves as a venue where patients can undergo videostroboscopic laryngeal examinations administered by subspecialty consultants. The Unit provides both diagnostic and therapeutic services for disorders of the larynx. Recent developments include in the involvement of our partner speech pathologists, who have contributed to a multidisciplinary approach in addressing speech and swallowing disorders.
Cochlear Implantation and Bone Anchored Hearing Aids
The Department is able to help qualified patients with hearing impairments by implanting advanced hearing apparatuses such as cochlear implants (CI) and bone anchored hearing aids (BAHA). The present Dean of the UPCM, Dean Charlotte Chiong, MD, PhD, helped pioneer cochlear implantation in the Philippines. Annually, the department does around 20 of these procedures.
CO2 Laser and KTP Laser Surgeries
Transoral laser microsurgery for benign and malignant conditions of the larynx has been one of the additional services provided by the department. It is an endoscopic approach to tumors with the use of either a CO2 or KTP laser to ablate or vaporize a lesion. It is minimally invasive and allows better surgical precision during resection. The laser has also been used in treatment of certain otologic conditions like glomus tympanicum and also has applications in the management of some vascular lesions.
Endoscopic Endonasal Approaches to the Skull Base
With the availability of the latest equipment for nasal endoscopy and skull base surgery such as HD endocameras, endoscopes, complete array of instrumentation and intraoperative surgical navigation systems, anterior skull base surgeries such as pituitary adenomas are performed endoscopically through the nose in collaboration with Neurosurgery.
Microvascular Reconstructive Surgery
Surgical resection of head and neck cancers and removal of large tumors may cause significant cosmetic and functional deformities among patients, thus requiring reconstruction to restore form and function. Aside from regional flaps, the Department is also able to do reconstruction with free flaps through microvascular surgery. It has proven to be very reliable for repair of defects and has the advantages of allowing surgeons not to compromise resection margins, can be completed in a single stage and allows a two-team approach during surgery.
Transoral Robotic Surgery
The arrival of the Da Vinci Surgical System in the Philippine General Hospital has further expanded the possibilities for surgical access via Transoral Robotic Surgery (TORS). Robotic surgery has allowed for safe and precise surgical options especially in conditions like oral and oropharyngeal carcinomas and obstructive sleep apnea.

Ward 10
Ward 10 of the Philippine General Hospital has a 42-bed capacity (39 adult beds, 3 pediatric beds), divided among five major services. Aftereffects of the COVID-19 pandemic on the hospital, however, resulted in bed distribution changes. Currently, the Department has a 17-bed (15 adult, 2 pediatric) allocation, with plans to return to or expand from the existing capacity.

Outpatient Clinic
The Department’s Outpatient Clinic, located in the Outpatient Department Building of UP-PGH, is open five days a week and provides comprehensive Otolaryngology services. General Clinics are held daily, with subspecialty clinics assigned on specific days of the week. Clinics are manned by residents and are supervised by subspecialty and medical specialist consultants.
Major Operating Rooms
The Department provides comprehensive surgical care, centered at the Major Operating Room Complex of UP-PGH. Three dedicated charity operating rooms are available for the Department’s use, with additional rooms afforded for pay/private cases. All trainee surgical cases are decked to consultants for guidance in management, and supervision is mandatory for teaching procedures and more complicated cases.
Emergency Room
The Otolaryngology - Head and Neck Surgery area of the UP-PGH emergency room is equipped in handling all urgent and emergent ORL-HNS conditions - acute pain, infections, foreign bodies in the upper airway and aerodigestive tract, upper airway bleeding, traumatic injuries, tumor complications, and all manners of upper airway compromise. Resident trainees and rotating UPCM students are on duty, with both junior and senior consultants having dedicated schedules for supervision.
The Department of Otolaryngology - Head and Neck Surgery of the UP-PGH is at the forefront of research in the field of ear, nose, throat disorders and head and neck conditions. With a strong commitment to advancing clinical knowledge, improve patient care and strengthen public health policies related to these disorders, the department’s faculty actively engages in diverse and impactful research areas.
Key Research Areas:
1. Otology, Neurotology, and Audiology
- Studies on hearing loss prevalence and risk factors in different population groups, including occupational hearing loss and ototoxicity
- Research on genetic and epigenetic determinants of hearing loss
- Outcomes of aural rehabilitation in children with hearing loss
- Studies on auditory screening techniques to improve early detection of hearing impairment
2. Rhinology, Sinus Disorders and Skull Base Tumors
- Studies on the epidemiology and management of chronic rhinosinusitis and nasal polyps
- Studies on olfactory dysfunction and its correlation with infectious diseases, such as COVID-19
- Research on skull base masses and surgical interventions to optimize treatment outcomes
3. Laryngology, Bronchoesophagology, Voice and Swallowing Disorders
- Research on voice disorders and phonosurgeries
- Studies on swallowing disorders aimed at improving diagnosis and treatment strategies
- Studies on laryngeal pathologies and laser treatment options
4. Head and Neck Oncology
- Studies on early detection, biomarkers and treatment outcomes of head and neck cancers
- Investigations into quality of life, functional outcomes and post treatment rehabilitation of head and neck cancer patients
- Outcomes of reconstructive free flap surgery
5. Craniomaxillofacial Fractures and Disorders and Prosthetics
- Innovation studies to improve surgical outcomes in the management of facial fractures
- Research on biomaterials and custom prosthetic reconstruction for craniofacial defects
- Studies on 3D printing and computer-assisted design for patient-specific implants
- Functional and aesthetic outcomes of maxillofacial reconstructive surgery
6. Sleep-Related Breathing Disorders
- Studies on screening tools and surgical and non-surgical options for sleep-disordered breathing
- Studies on the epidemiology and risk factors for obstructive sleep apnea in different populations
Department of Otolaryngology - Head and Neck Surgery
University of the Philippines College of Medicine –
2nd Floor, Main Building, Philippine General Hospital
Taft Avenue, Manila 1000
REPUBLIC OF THE PHILIPPINES
TELEPHONE: 8554-8400 loc. 2152/ 85548467
EMAIL: orl.uppgh@up.edu.ph
Facebook: https://fb.me/UPCMPGHORL
